Published 2025-04-10
Keywords
- GIS,
- Urban Health,
- Kolkata,
- India,
- Built Environment
- Spatial Risk Analysis,
- Environmental Health,
- Urban Planning ...More
How to Cite
Copyright (c) 2025 Anu Rai, Kasturi Adhikary, Debisha Ghosh Ghosh, Mohor Samaddar Samaddar, Hrileena Chowdhury Chowdhury, Sayanika Si

This work is licensed under a Creative Commons Attribution 4.0 International License.
Accepted 2025-04-08
Published 2025-04-10
Abstract
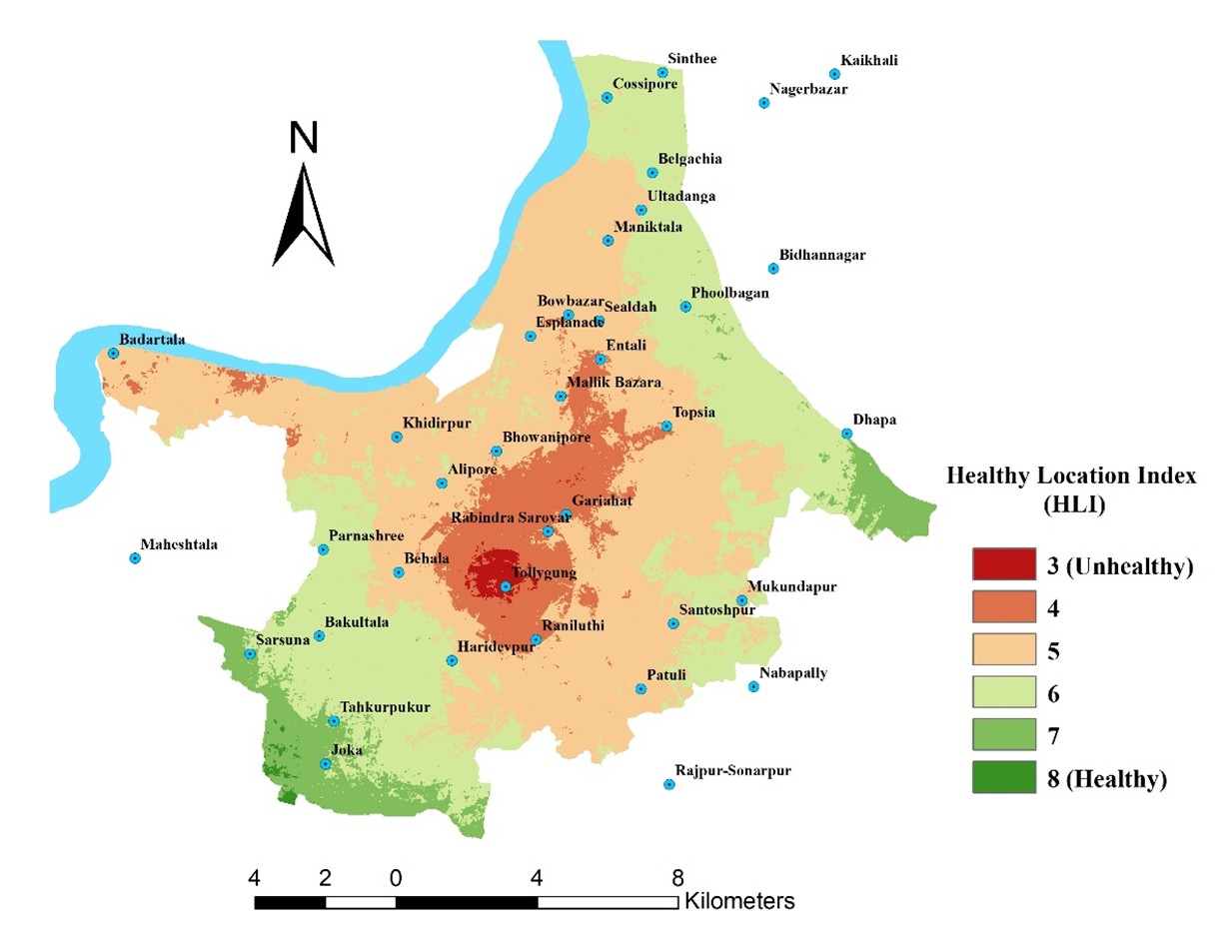
Urban health outcomes are shaped by the complex interplay of environmental, social, and spatial factors. This study develops a Healthy Location Index (HLI) to assess spatial health risks by integrating health-promoting (HPSVs) and health-restraining (HRSVs) spatial variables using geospatial analysis and the Analytic Hierarchy Process (AHP). Taking Kolkata, India, as a case study, the HLI incorporates factors such as green and blue spaces, built-up density, air quality, and the distribution of alcohol and fast-food outlets to create a spatial model of urban health. The study utilizes remotely sensed and administrative datasets (e.g., Landsat-derived NDVI, NDBI, NDWI, Point-of-Interest data) and validates the HLI against COVID-19 containment zones (June 2020–January 2021) using Receiver Operating Characteristic (ROC) analysis. Results indicate that areas with high HLI scores—characterized by greater access to green spaces and lower exposure to environmental stressors—were less likely to be containment zones, suggesting a meaningful relationship between spatial health factors and urban resilience. However, the study acknowledges potential confounding variables, such as socioeconomic disparities, population density, and healthcare accessibility, which may influence health outcomes. The findings underscore the global applicability of the HLI framework in urban planning, public health policy, and epidemiological risk assessment, offering a scalable model for cities facing rapid urbanization and environmental challenges.
Highlights:
- Proposed a scalable HLI framework with global implications for urban planning and targeted health interventions.
- Validation using COVID-19 containment zones and ROC analysis, demonstrating the utility of HLI in predicting health-risk areas.
- Policy implications for global urban planning and health interventions, emphasizing the need for improved green space access and environmental risk mitigation.
Downloads
References
- Arcaya, M. C., Arcaya, A. L., & Subramanian, S. V. (2016). Inequalities in health: Definitions, concepts, and theories. Global Health Action, 9(1), 1-12. https://doi.org/10.3402/gha.v9.27106
- Banay, R. F., James, P., Hart, J. E., Kubzansky, L. D., Spiegelman, D., Okereke, O. I., ... & Laden, F. (2017). Green space and mortality in a US pro-spective cohort study of women. Environmental Health Perspectives, 125(8), 1-8. https://doi.org/10.1289/EHP1663
- Banay, R. F., James, P., Hart, J. E., Kubzansky, L. D., Spiegelman, D., Okereke, O. I., Spengler, J. D., & Laden, F. (2019). Greenness and depression incidence among older women. Environmental Health Perspectives, 127(2), 27001. https://doi.org/10.1289/EHP1229
- Beyer, K. M., Kaltenbach, A., Szabo, A., Bogar, S., Nieto, F. J., & Malecki, K. M. (2014). Exposure to neighborhood green space and mental health: Evidence from the Survey of the Health of Wisconsin. International Journal of Environmental Research and Public Health, 11(3), 3453–3472. https://doi.org/10.3390/ijerph110303453
- Block, J. P., Scribner, R. A., & DeSalvo, K. B. (2004). Fast food, race/ethnicity, and income: A geographic analysis. American Journal of Preventive Medicine, 27(3), 211–217. https://doi.org/10.1016/j.amepre.2004.06.007
- Central Pollution Control Board. (2018). Air quality trends and action plan for control of air pollution from particulate matter. Retrieved from https://cpcb.nic.in
- Centre for Science and Environment (CSE). (2020). State of India's Environment Report.
- Chen, J., Yang, S., Li, H., Zhang, B., & Lv, J. (2020). Research on geographical environment unit division based on the method of natural breaks (Jenks). International Journal of Geo-Information, 9(9), 1-15. https://doi.org/10.3390/ijgi9090502
- Chrisinger, B.W., King, A.C. Stress experiences in neighborhood and social environments (SENSE): a pilot study to integrate the quantified self with citizen science to improve the built environment and health International Journal of Health Geographics 17, 17 (2018). https://doi.org/10.1186/s12942-018-0140-1
- Clark, L. P., Zilber, D., Schmitt, C., et al. (2024). A review of geospatial exposure models and approaches for health data integration. Journal of Exposure Science & Environmental Epidemiology. https://doi.org/10.1038/s41370-024-00712-8
- Cobb, L. K., Appel, L. J., Franco, M., Jones-Smith, J. C., Nur, A., & Anderson, C. A. (2015). The relationship between the local food environment and obesity: A systematic review of methods, study quality, and results. Obesity, 23(7), 1331-1344. https://doi.org/10.1002/oby.21118
- De, S., Rai, A. (2024). Spatial Heterogeneity and Pandemic Dynamics: Geospatial Insights from Kolkata During Post-Lockdown COVID-19 Spread and Management. In: Rai, A., Karmakar, S., Chatterjee, S., Pandey, J.K. (eds) Contemporary Social Physics. Springer Geography. Springer, Cham. https://doi.org/10.1007/978-3-031-77596-3_14
- Diez Roux, A. V., & Mair, C. (2010). Neighborhoods and health. Annals of the New York Academy of Sciences, 1186(1), 125-145. https://doi.org/10.1111/j.1749-6632.2009.05333.x
- Economist Intelligence Unit. (2022). Global Liveability Index. Retrieved from https://www.eiu.com
- Faka, A., Chalkias, C., Damigou, E., Chrysohoou, C., Barkas, F., Dalmyras, D., Kyrilli, K., Pitsavos, C., Liberopoulos, E., Tsioufis, C., Sfikakis, P., & Panagiotakos, D. (2024). Exploring Spatiotemporal Patterns of Cardiovascular Disease in Greece: Insights from the ATTICA Study (2002-2022). European Journal of Geography, 15(4), 271–280. https://doi.org/10.48088/ejg.a.fak.15.4.271.280
- Fraser, L. K., Edwards, K. L., Cade, J., & Clarke, G. P. (2010). The geography of fast-food outlets: A review. International Journal of Environmental Research and Public Health, 7(5), 2290–2308. https://doi.org/10.3390/ijerph7052290
- Frumkin, H. (2003). Healthy places: Exploring the evidence. American Journal of Public Health, 93(9), 1451–1456. https://doi.org/10.2105/ajph.93.9.1451
- Ganasegeran, K., Abdul Manaf, M. R., Safian, N., Waller, L. A., Abdul Maulud, K. N., & Mustapha, F. I. (2024). GIS-based assessments of neighbor-hood food environments and chronic conditions: An overview of methodologies. Annual Review of Public Health, 45, 109–132. https://doi.org/10.1146/annurev-publhealth-101322-031206
- Gascon, M., Triguero-Mas, M., Martínez, D., Dadvand, P., Forns, J., Plasència, A., & Nieuwenhuijsen, M. J. (2015). Mental health benefits of long-term exposure to residential green and blue spaces: A systematic review. International Journal of Environmental Research and Public Health, 12(4), 4354–4379. https://doi.org/10.3390/ijerph120404354
- Gascon, M., Zijlema, W., Vert, C., White, M. P., & Nieuwenhuijsen, M. J. (2016). Outdoor blue spaces, human health and well-being: A systematic review of quantitative studies. International Journal of Hygiene and Environmental Health, 219(8), 879–893. https://doi.org/10.1016/j.ijheh.2017.08.004
- Gascon, M., Zijlema, W., Vert, C., White, M. P., & Nieuwenhuijsen, M. J. (2017). Outdoor blue spaces, human health and well-being: A systematic review of quantitative studies. International Journal of Hygiene and Environmental Health, 220(8), 1207–1221. https://doi.org/10.1016/j.ijheh.2017.08.004
- Haque, M. S., & Singh, R. B. (2017). Air pollution and human health in Kolkata, India: A case study. Climate, 5(4), 77. https://doi.org/10.3390/cli5040077
- Harpham, T., & Werna, E. (1996). Sustainable urban health in developing countries. Habitat International, 20(3), 421–429. https://doi.org/10.1016/0197-3975(96)00011- 2
- Kar, S., Chowdhury, S., Gupta, T., Hati, D., De, A., Ghatak, Z., Tinab, T., Rahman, I. T., Chatterjee, S., & RoyChowdhury, A. (2024). A study on the impact of air pollution on health status of traffic police personnel in Kolkata, India. Air, 2(1), 1–23. https://doi.org/10.3390/air2010001
- Kirkbride, J. B., Anglin, D. M., Colman, I., Dykxhoorn, J., Jones, P. B., Patalay, P., Pitman, A., Soneson, E., Steare, T., Wright, T., & Griffiths, S. L. (2024). The social determinants of mental health and disorder: Evidence, prevention and recommendations. World Psychiatry, 23(1), 58–90. https://doi.org/10.1002/wps.21160
- Lak, A., Shakouri Asl, S., & Maher, A. (2020). Resilient urban form to pandemics: Lessons from COVID-19. Medical Journal of the Islamic Republic of Iran, 34, 71. https://doi.org/10.34171/mjiri.34.71
- Lowe, M., Boulange, C., & Giles-Corti, B. (2014). Urban design and health: Progress to date and future challenges. Health Promotion Journal of Australia, 25(1), 14–18. https://doi.org/10.1071/HE13072
- Maji, K. J., Dikshit, A. K., & Deshpande, A. (2017). Assessment of city-level human health impact and corresponding monetary cost burden due to air pollution in India, taking Agra as a model city. Air Quality, Atmosphere & Health, 17(3), 8072. https://doi.org/10.4209/aaqr.2016.02.0067
- Manisalidis, I., Stavropoulou, E., Stavropoulos, A., & Bezirtzoglou, E. (2020). Environmental and health impacts of air pollution: A review. Fron-tiers in Public Health, 8, 14. https://doi.org/10.3389/fpubh.2020.00014
- Marek, L., Campbell, M., Epton, M., Kingham, S., & Storer, M. (2021a). The Healthy Location Index: A tool for community health improvement. Health & Place, 67, 102489. https://doi.org/10.1016/j.healthplace.2020.102489
- Marek, L., Hobbs, M., Wiki, J., et al. (2021b). The good, the bad, and the environment: Developing an area-based measure of access to health-promoting and health-constraining environments in New Zealand. International Journal of Health Geographics, 20(1), 16. https://doi.org/10.1186/s12942-021-00269-x
- Mas, J.-F., Soares Filho, B., Pontius, R. G., Farfán Gutiérrez, M., & Rodrigues, H. (2013). A suite of tools for ROC analysis of spatial models. ISPRS International Journal of Geo-Information, 2(3), 869–887. https://doi.org/10.3390/ijgi2030869
- Maulken, A., Alikhan, M., & Akhmetkal, M. (2023). Assessing the level of environmental health security affected by atmosphere pollution. Euro-pean Journal of Geography, 7(2), 72–84. https://eurogeojournal.eu/index.php/egj/article/view/395
- Mukhopadhyay, A. K., Deb, A. K., Chowdhury, G., Debnath, F., Samanta, P., Saha, R. N., Manna, B., Bhattacharya, M. K., Datta, D., Okamoto, K., Bhadra, U. K., & Dutta, S. (2019). Post-monsoon waterlogging-associated upsurge of cholera cases in and around Kolkata metropolis, 2015. Epidemiology and Infection, 147, e167. https://doi.org/10.1017/S0950268819000529
- Myerson, J. (2023, December 6). Concept and conspiracy: The 15-minute city in the spotlight. Oxford Institute of Population Ageing. https://www.ageing.ox.ac.uk/blog/Concept%20and%20Conspiracy%3AThe-15-minute-City-in-the-Spotlight
- Nath, B., Majumder, S., Sen, J., & Rahman, M. M. (2021). Risk analysis of COVID-19 infections in Kolkata Metropolitan City: A GIS-based study and policy implications. GeoHealth, 5(4), e2020GH000368. https://doi.org/10.1029/2020GH000368
- Nieuwenhuijsen, M. J. (2018). Urban and transport planning, environmental exposures, and health: New concepts, methods, and tools to im-prove health in cities. Environmental Health, 17(1), 1-10. https://doi.org/10.1186/s12940-018-0389-7
- Ozdenerol, E. (2016). Spatial health inequalities: Adapting GIS tools and data analysis (1st ed.). CRC Press. https://doi.org/10.1201/9781315371894
- Perdue, W. C., Stone, L. A., & Gostin, L. O. (2003). The built environment and its relationship to the public’s health: The legal framework. Ameri-can Journal of Public Health, 93(9), 1390–1394. https://doi.org/10.2105/ajph.93.9.1390
- Pineo, H., Glonti, K., Rutter, H., Zimmermann, N., Wilkinson, P., & Davies, M. (2018). Urban health indicator tools of the physical environment: A systematic review. Journal of Urban Health, 95(5), 613–646. https://doi.org/10.1007/s11524-018-0228-8
- Rai, A. (2019). Management of medical tourism in Kolkata: Strategies and evaluation. In Medical tourism in Kolkata, Eastern India (pp. 131–145). Global Perspectives on Health Geography. Springer. https://doi.org/10.1007/978-3-319-73272-5_8
- Richardson, E. A., Hill, S. E., Mitchell, R., Pearce, J., & Shortt, N. K. (2015). Is local alcohol outlet density related to alcohol-related morbidity and mortality in Scottish cities? Health & Place, 33, 172–180. https://doi.org/10.1016/j.healthplace.2015.02.014
- Routh, D., Rai, A., & Bhunia, G. S. (2023). Post-lockdown spatiotemporal pattern of COVID clustering in North 24 Parganas, West Bengal, India. Spatial Information Research, 31(1), 101–112. https://doi.org/10.1007/s41324-022-00483-0
- Roy, S., Bose, A., Majumder, S., Roy Chowdhury, I., Abdo, H. G., Almohamad, H., & Abdullah Al Dughairi, A. (2022). Evaluating urban environ-ment quality (UEQ) for Class-I Indian city: an integrated RS-GIS based exploratory spatial analysis. Geocarto International, 38(1). https://doi.org/10.1080/10106049.2022.2153932
- Saaty, T., & Kearns, K. (1985). Analytical planning: The organization of systems. Pergamon Press.
- Sarkar, C., Webster, C., & Gallacher, J. (2018). Residential greenness and prevalence of major depressive disorders: A cross-sectional, observa-tional, associational study of 94,879 adult UK Biobank participants. The Lancet Planetary Health, 2(4), e162–e173. https://doi.org/10.1016/S2542-5196(18)30051-2
- Sen, S., & Guchhait, S. K. (2021). Urban green space in India: Perception of cultural ecosystem services and psychology of situatedness and con-nectedness. Ecological Indicators, 130, 107338. https://doi.org/10.1016/j.ecolind.2021.107338
- Spiroska, J., Rahman, A. & Pal, S. Air Pollution in Kolkata: An Analysis of Current Status and Interrelation between Different Factors. SEEU Review, 2011, Sciendo, vol. 8 no. 1, pp. 182-214. https://doi.org/10.2478/v10306-012-0012-7
- Thornton, L. E., Lamb, K. E., & Ball, K. (2016). Fast food restaurant locations according to socioeconomic disadvantage, urban-regional locality, and schools within Victoria, Australia. SSM - Population Health, 2, 1–9. https://doi.org/10.1016/j.ssmph.2015.12.001
- Twohig-Bennett, C., & Jones, A. (2018). The health benefits of the great outdoors: A systematic review and meta-analysis of greenspace expo-sure and health outcomes. Environmental Research, 166, 628-637. https://doi.org/10.1016/j.envres.2018.06.030
- van den Berg, M., Wendel-Vos, W., van Poppel, M., Kemper, H., van Mechelen, W., & Maas, J. (2015). Health benefits of green spaces in the living environment: A systematic review of epidemiological studies. Urban Forestry & Urban Greening, 14(4), 806–816. https://doi.org/10.1016/j.ufug.2015.07.008
- World Health Organization. (1985). Healthy Cities: Promoting Health in the Urban Context. WHO Europe.
- World Health Organization. (2020). Global air quality guidelines. Geneva: World Health Organization.
- Zhou, Y., Lengerke, T., & Dreier, M. (2021a). Urban health indicators and indices: Current trends in research and practice. Journal of Urban Health, 98(1), 1-15. https://doi.org/10.1007/s11524-020-00485-7
- Zhou, Y., von Lengerke, T., & Dreier, M. (2021b). Comparing different data sources by examining the associations between surrounding green-space and children's weight status. International Journal of Health Geographics, 20, 24. https://doi.org/10.1186/s12942-021-00278-w




